Are you one of the many people unknowingly living or working in water damaged building? Did you know it may be dramatically affecting your health? It's estimated that indoor air pollutants, including mold and mycotoxins may be contributing to more than 50% of our patient's illnesses. Typically we think of smog, smoke, and outdoor pollution as detrimental to our health but indoor air quality may be an even bigger risk to your health. Many patients are unaware that a toxic home or workplace is contributing to their symptoms.
Exposure to water-damaged indoor environments is associated with exposure to molds. The most common types of mold that are found indoors include Cladosporium, Penicillium, Alternaria, and Aspergillus. Stachybotrys chartarum (sometimes referred to as "toxic black mold") is a greenish-black mold, which grows on household surfaces that have high cellulose content, such as wood, fiberboard, gypsum board, paper, dust, and lint and is usually an indicator that there has been elevated moisture present or previous water damage.
Some molds secrete mycotoxins, that can be measured in the urine, such as ochratoxin, aflatoxin, and trichothecenes. Exposure to mold and mold components is well known to trigger inflammation, allergies and asthma, oxidative stress, and immune dysfunction in both human and animal studies. Mold spores, fungal fragments, and mycotoxins can be measured in the indoor environments of moldy buildings and in humans who are exposed to these environments. Most of the time, we are exposed to molds, like stachybotrys, through the skin contact, through ingestion, and by inhalation. Most common are reports of exposure involve water-damaged homes, schools, office buildings, court houses, hospitals, and hotels. It's estimated that as many as 25% of buildings in the US have had some sort of water damage. Molds have the ability to produce various symptoms, such as skin rashes, respiratory distress, various types of inflammation, cognitive issues, neurological symptoms, and immune suppression. The most common symptoms associated with mold exposure are allergic rhinitis and new onset asthma.
How do you know if you've been exposed to mold or mycotoxins?
Top Symptoms Associated with Mycotoxin-Associated Illness:
- Fatigue and weakness
- Headache, light sensitivity
- Poor memory, difficult word finding
- Difficulty concentration
- Morning stiffness, joint pain
- Unusual skin sensations, tingling and numbness
- Shortness of breath, sinus congestion or chronic cough
- Appetite swings, body temperature regulation,
- Increased urinary frequency or increased thirst
- Red eyes, blurred vision, sweats, mood swings, sharp pains
- Abdominal pain, diarrhea, bloating
- Tearing, disorientation, metallic taste in mouth
- Static shocks
- Vertigo, feeling lightheaded
Checklist that might indicate mold exposure or mold sensitivity (from ECH website)
- Do musty odors bother you?
- Have you worked or lived in a building where the air vents or ceiling tiles were discolored?
- Have you noticed water damage or discoloration elsewhere?
- Has your home been flooded?
- Have you had leaks in the roof?
- Do you experience unusual shortness of breath?
- Do you experience recurring sinus infections?
- Do you experience recurring respiratory infections and coughing?
- Do you have frequent flu-like symptoms?
- Do your symptoms worsen on rainy days?
- Do you have frequent headaches?
- Are you fatigued and have a skin rashes?
How do I Treat Mold/mycotoxin Exposure?
- Remove yourself from the contaminated environment (don't even think about going on to other treatments until you get out of the contaminated environment)
- Avoid exposure to porous items (paper, clothing, etc) from the moldy environment.
- Use clay, charcoal, cholestyramine or other binders to bind internal mycotoxins
- While you are using binders, you must maintain normal bowel function and avoid constipation. You can add magnesium citrate, buffered C powder, or even gentle laxatives if needed but constipation is the enemy of detoxification!
- Treat colonizing molds/fungal infections in the body
- Common locations of colonization include sinuses, gut, bladder, vagina, lungs
- Test and treat for candida overgrowth - living in an environment with mold leads to immune dysregulation that allows candida to overgrow in the body
- Enhance detoxification support
- Some common supplements used to aid detox are liposomal glutathione, milk thistle, n-acetylcysteine, alpha lipoid acid, glycine, glutamine, and taurine. Methylation support is also key and involves optimal levels of methylcobalamin (B12), methyl-folate, B6, riboflavin, and minerals
- Invest in a high quality air filter and home and at work, like Austin Air or EL Faust
- Avoid common mycotoxin containing foods:
- Corn, wheat, barley, rye, peanuts, sorghum, cottonseed, some cheeses, and alcoholic beverages such as wine and beer. Others include oats, rice, tree nuts pistachios, brazil nuts, chiles, oil seeds, spices, black pepper, dried fruits, figs, coffee, cocoa, beans, bread.
Other Treatment Options
- Follow Dr. Jill's Low Mold Diet - many patients to well on a paleo, grain-free diet since grains are often contaminated with mycotoxins and molds
- Sublingual immunotherapy (SLIT)
- Anti-fungal herbs and medications
- Infared sauna
- Detoxification support - oral and IV
- Remediation procedures for environment and belongings
- Create a "safe" place, with little potential for mold/allergens and great filtration system - this could be a bedroom or other room that is mold and chemical free
- Some patients benefit from IV immunoglobulin therapy (IVIg)
Chart from article in Townsend Letter July 2014 that explains sources and binders for common mycotoxins: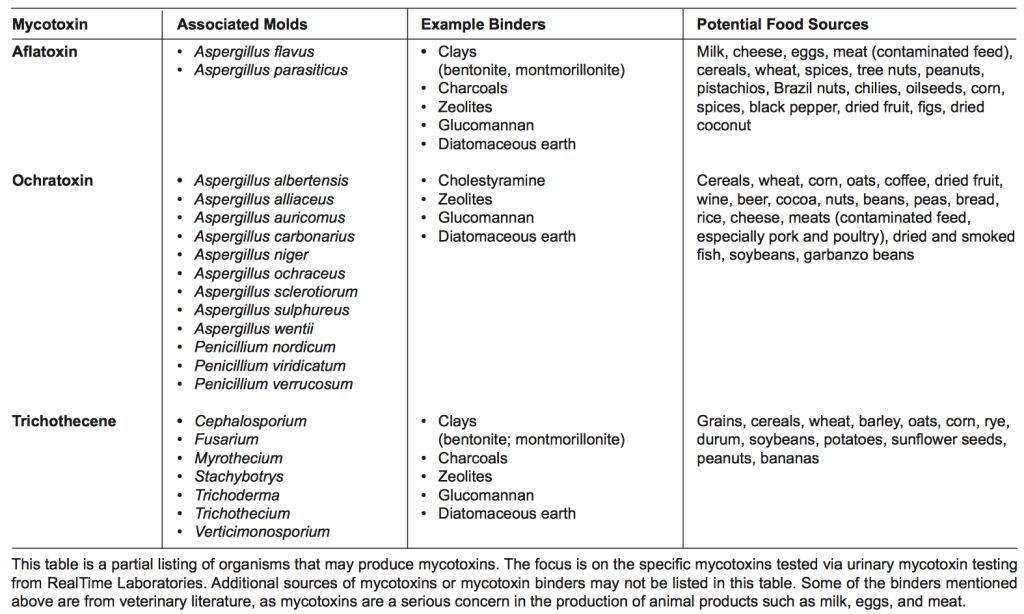
More Helpful Resources:
- Guidance for Clinicians on the Recognition and Management of Health Effects Related to Mold Exposure and Moisture Indoors
- A Review of the Mechanism of Injury and Treatment Approaches for Illness Resulting from Exposure to Water-Damaged Buildings, Mold, and Mycotoxins
- Chronic Inflammatory Response Syndrome - Dr. Berndtson
- Slide Presentation on Mold Toxicity
- Paradigm Change - information on role of mold toxins in Chronic Neuroimmune Disease
- Real Time Labs - Urinary Mycotoxin Testing
- Fungal spore DNA detectible in tissue and body fluids of patients exposed to moldy buildings
- Stachybotrys chartarum: Review of Toxicology Literature





