Mast Cell Activation Syndrome (MCAS): When Histamine Goes Haywire...
Mast cells are present in most tissues throughout the human body, especially connective tissue, skin, intestinal lining cardiovascular system, nervous system, and reproductive organs. They are part of the allergic response designed to protect us from threat and injury. When the body is exposed to a perceived threat, the mast cells secrete chemical mediators, such as histamine, interleukins, prostaglandins, cytokines, chemokine and various other chemicals stored in the cytoplasm of the cell. These chemical messengers produce both local and systemic effects, such as increased permeability of blood vessels (inflammation and swelling), contraction of smooth muscle (stomach cramps and heart palpitations), and increase mucous production (congestion, sneezing, etc). Historically, we thought of mast cells only in relation to an allergic or anaphylactic response. We now know they play a profound role in immune activation, development of autoimmunity and many other disorders, such as POTS (postural orthostatic tachycardia syndrome). Sadly we are seeing a large increase in patients presenting with mast cell disorders and MCAS. I believe it is in part do to the onslaught of more pervasive environmental toxins, molds and chemicals.
Withouts mast cells, we would not be able to heal from a wound. They protect us from injury and help the body to heal. Unforunately, overactive mast cells can cause a variety of serious symptoms.
Symptoms of overactive mast cells may include:
- skin rashes/hives
- swelling/edema
- flushing
- itching
- abdominal pain
- nausea/vomiting
- diarrhea
- wheezing
- shortness of breath
- heart palpitations
- anxiety, difficulty concentrating
- headaches
- brain fog
- low blood pressure
- fatigue
Mast cell activation syndrome (MCAS) is a condition symptoms involving the skin, gastrointestinal, cardiovascular, respiratory, and neurologic systems. It can be classified into primary (clonal proliferation or mastocytosis), secondary (due to a specific stimulus), and idiopathic (no identifiable cause). Proposed criteria for the diagnosis of MCAS included episodic symptoms consistent with mast cell mediator release affecting two or more organ systems with hives, swelling, flushing, nausea, vomiting, diarrhea, abdominal pain, low blood pressure, fainting, heart palpitations, wheezing, red eyes, itching, and/or nasal congestion. For a diagram of all of the varied symptoms histamine can cause, click here.
Triggers may be medications, foods, supplements, hormones, opioids, stressors (physical or emotional), cold temperature, heat, pressure, noxious odors, chemicals, insect bites, trauma or environmental toxins.
We commonly see mast cell activation syndromes associated with CIRS (chronic inflammatory response syndrome) in response to biotoxins, such as mold, inflammagens, and lyme-related toxins.
Low MSH and Mast Cell Disorders?
As mentioned above, we frequently see histamine intolerance and MCAS in patients with mold-related CIRS (chronic inflammatory response syndrome). It is interesting to note that a common finding in CIRS is low MSH. According to this study in the Journal of Investigative Dermatology, alpha-MSH plays an immunomodulatory role during inflammatory and allergic reactions of the skin. In addition, there is evidence that MSH induces mast-cell apoptosis (cell death).
Definition of Mast Cell Activation Syndrome (MCAS)
- Typical clinical symptoms as listed above
- Increase in serum tryptase level or an increase in other mast cell derived mediators, such as histamine or prostaglandins (PGD2), or their urinary metabolites,
- Response of symptoms to treatment
- Mast cells can be activated by both direct and indirect mechanisms as a result of exposure of the host to pathogens.
Diseases Associated with Mast Cell Activation Syndrome (MCAS)
- Allergies and Asthma
- Autism
- Autoimmune diseases (Hashimoto's thyroiditis, systemic lupus, multiple sclerosis, bullous pemphigoid, rheumatoid arthritis and others.Eczema
- Celiac Disease
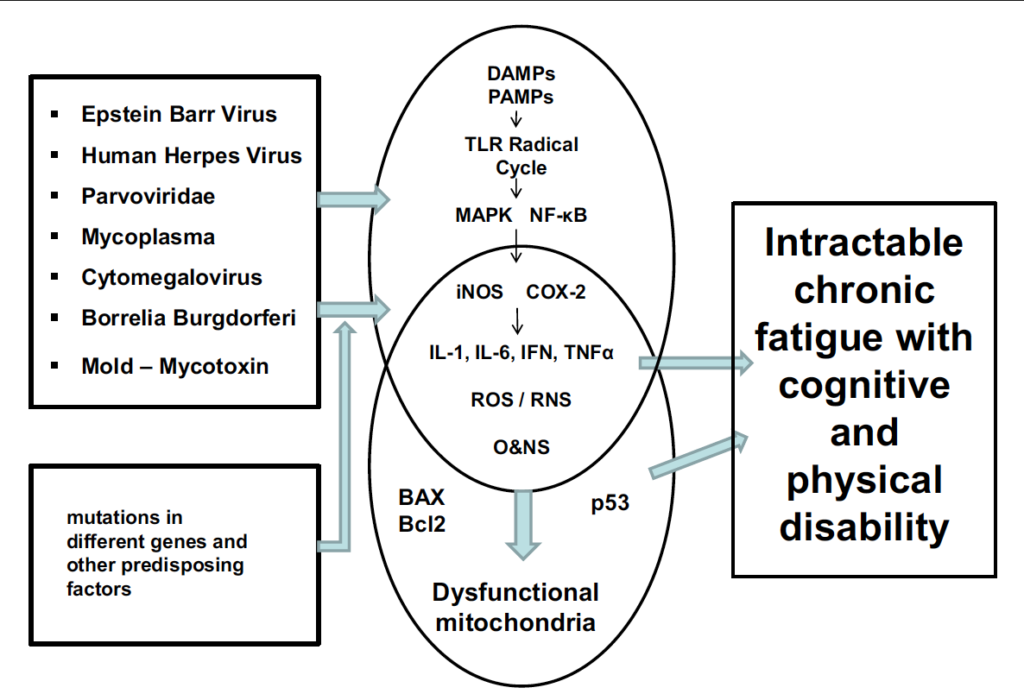
- Chronic Fatigue Syndrome
- CIRS (chronic inflammatory response syndrome)
- Eosinophilic Esophagitis
- Fibromyalgia
- Food Allergy and Intolerances
- Gastroesophageal reflux (GERD)
- Infertility (mast cells in endometrium may contribute to endometriosis)
- Interstitial Cystitis
- Irritable Bowel Syndrome (IBS)
- Migraine Headaches
- Mood disorders - anxiety, depression, and insomnia
- Multiple Chemical Sensitivities
- POTS (postural orthostatic hypotension)
- Mast cells are known to be the primary responders in allergic reactions, orchestrating strong responses to minute amounts of allergens. Several recent observations indicate that they may also have a key role in coordinating the early phases of autoimmune diseases, particularly those involving auto-antibodies.
Lab Tests for Mast Cell Activation Syndrome (MCAS)
- Lab tests specific to mast cell activation for suspected MCAS may include:
- Serum tryptase (most famous mast cell mediator)
- Serum chromogranin A
- Plasma histamine
- Plasma PGD2 (chilled)
- Plasma heparin (chilled)
- Urine for PGD2 (chilled)
- PGF2a
- N-methylhistamine
- Tryptase is the most famous mast cell mediator. Serum tryptase value is usually normal in MCAS patients, but sometimes it is elevated. Tryptase values that show an increase of 20% + 2 ng/ml above the baseline level are considered diagnostic for MCAS.
- Chromogranin A is a heat-stable mast cell mediator. High levels can suggest MCAS, but other sources must first be ruled out, such as heart failure, renal insufficiency, neuroendocrine tumors and proton pump inhibitor (PPI) use.
- Heparin is a very sensitive and specific marker of mast cell activation. However, due to its quick metabolism in the body, it is very difficult to measure reliably.
- N-methylhistamine is usually measured in a 24 hour urine test to account for the variability in release over the course of the day.
- Prostaglandin D2 is produced by several other cell types, but mast cell release is responsible for the dominant amount found in the body. PGD2 is less stable than histamine and metabolized completely in 30 minutes.
- Other less specific mast cell mediators that are sometimes abnormal in MCAS patients include Factor VIII, plasma free norepinephrine, tumor necrosis factor alpha, and interleukin-6.
Treatments to reduce MCAS symptoms and lower histamine
- H1 Blockers
- hydroxyzine, doxepine, diphenhydramine, cetirizine, loratadine, fexofenadine
- H2 Blockers
- Famotidine (Pepcid, Pepcid AC)
- Cimetidine (Tagamet, Tagamet HB)
- Ranitidine (Zantac)
- Leukotriene inhibitors
- Montelukast (Singulair)
- Zafirlukast (Accolate)
- Mast cell stabilizers -
- Cromolyn
- Ketotifen
- Hyroxyurea
- Tyrosine kinase inhibitors - imatinib
- Natural anti-histamines and mast-cell stabilizers
- Ascorbic Acid
- Quercetin
- Vitamin B6 (pyridoxal-5-phosphate)
- Omega-3 fatty acids (fish oil, krill oil)
- Alpha Lipoic Acid
- N-acetylcysteine (NAC)
- Methylation donors (SAMe, B12, methyl-folate, riboflavin)
- Certain probiotics decrease histamine production
- Lactobacillus rhamnosus and bifidobacter species
- DAO Enzymes with meals - Xymogen HistDAO or Histamine
- Decrease consumption of high histamine foods (more on histamine-restricted diet)
- Avoid alcoholic beverages
- Avoid raw and cured sausage products such as salami.
- Avoid processed or smoked fish products. Use freshly caught seafood instead.
- Avoid pickles
- Avoid citrus fruits.
- Avoid chocolate
- Avoid nuts
- Avoid products made with yeast and yeast extracts
- Avoid soy sauce and fermented soy products
- Avoid black tea and instant coffee
- Avoid aged cheese
- Avoid spinach in large quantities
- Avoid tomatoes, ketchup and tomato sauces
- Avoid artificial food colorings & preservatives
- Avoid certain spices: cinnamon, chili powder, cloves, anise, nutmeg, curry powder, cayenne pepper
Specific Symptom Treatment in MCAS
- Headache⇒ paracetamol; metamizole; flupirtine
- Diarrhea⇒ colestyramine; nystatin; montelukast; ondansetron
- Colicky abdominal pain ⇒ metamizole; butylscopolamine
- Nausea⇒ metoclopramide; dimenhydrinate; 5-HT3 receptor inhibitors; icatibant
- Respiratory symptoms (mainly increased production of viscous mucus and obstruction with compulsive throat clearing) ⇒ montelukast; acute: short-acting albuterol
- Gastric complaints⇒ proton pump inhibitors
- Osteoporosis, bone pain⇒ biphosphonates, Vitamin D plus calcium
- Non-cardiac chest pain⇒ H2-histamine receptor antagonist; proton pump inhibitors
- Tachycardia⇒ verapamil; AT1-receptor antagonists; ivabradin
- Neuropathies ⇒ a-lipoic acid
- Interstitial cystitis⇒ pentosan, amphetamines
- Sleep-onset insomnia/sleep-maintenance insomnia⇒ triazolam/oxazepam
- Conjunctivitis⇒ preservative-free eye drops with glucocorticoids for brief course
- Elevated prostaglandin levels, persistant flushing⇒ incremental doses of acetylsalicylic acid (50-350 mg/day; extreme caution because of the possibility to induce mast cell degranulation)
References
- Mast Cell Activation Syndrome, A Review
- Mast cell activation disease: a concise practical guide for diagnostic workup and therapeutic options
- Presentation, Diagnosis and Management of Mast Cell Activation Syndrome by Dr. Afrin
- Histamine and Gut Immune Mucosal Regulation
- Dr. Theoharides presents “Mast Cell Disorders”
- Diagram of Histamine Symptoms
- Mast Cell Aware
- A Tale of Two Syndromes
- Mold Histamine Connection